Welcome to Dental and Eye Hospital
Dr. Puran Chand Memorial Eye & Dental Hospital Is A Known Superspeciality Centre For The Dental & Eye Care. It Offers World Class Modern Diagnostic, Therapeutic And Rehabilitative Eye & Dental Treatments To The Twin City At A Very Reasonable Cost.
It Was Established In 2002 By Dr. Punit Bansal & Dr. Ruchi Bansal With Soul Intent To Provide High-Quality Dental & Eye Care At A Low Cost.
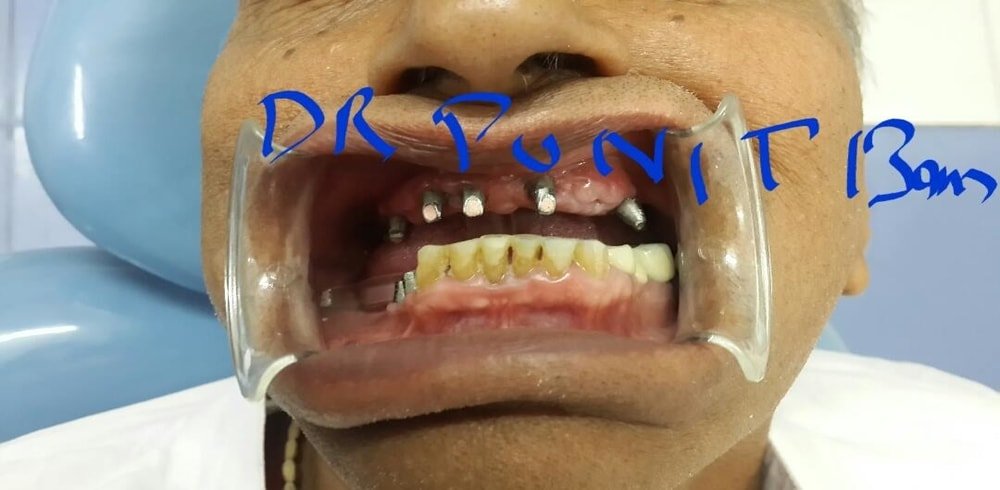
Dr Punit Bansal Acquired His Bds Degree From The Oldest & Prestigious Govt. Dental College Rohtak (Haryana) In 1996. He Did His Postgraduation From Dav Centenury Dental College & Hospital Yamuna Nagar In Deptt. Of Conservative Dentistry & Endodontics As 1st Batch Of Postgradutes In 2001. After Doing His Masters He Started His Private Practice At Dental Clinic Of His Grand Father Late Dr. Puran Chand Gupta Who Was The Poineers In This Profession In The Twin City. His Grand Father Served The Twin City For More Than 65yrs Passing The Batton To Dr Punit Bansal Who Has Earned A Reputation Of Adopting The Latest Technology & Adhering To Ethical Practice In The Field Of Dentistry .he Was First To Introduce Digital Opg And Dental Implants To This Town In The Year 2008 When No Dentist Thought Of Such Advancements In This Field. He Took His Dental Implant Education From The Most Popular Maxicourse Run By American Academy Of Implant Dentistry (Aaid) Usa Under The Esteemed Guidance Of Dr Shankaar Iyer, The World Known Oral Implantologist And Mentor. During His Practice Now He Has More 200 Successsful Cases Of Different Form Of Dental Implant Rehabilitative Options.


Dr Ruchi Bansal Graduated From Govt Medical College Bhopal In The Year 1998 And Did Her Post Garduation From Govt. Medical College Amritsar In The Field Of Ophthlmology.
She Specialised In The Field Of Daibetic Retinopathy And Medial Retina From The Prestigious Aravind Eye Hospital, Madurai. She Further Did Her Fellwoship In Advanced Phaco Emulsification From Venu Eye Institute, New Delhi.
She Being An Enterpuerner Has Alll The Latest Eye Equipments Like Oct ,nct ,autoref And The Latest Johnson & Johnson Soverign Compaque Phaco Machine In Her Hospital To Treat All The Eye Problems At The Best . She Also Arranges Rotary Camps Regulary And Has Operated More Then 4000 Patients For Free In The Different Rotary Camps.
Why Dr. Punit Bansal's Dental and Eye Hospital
Dental Facilities Available
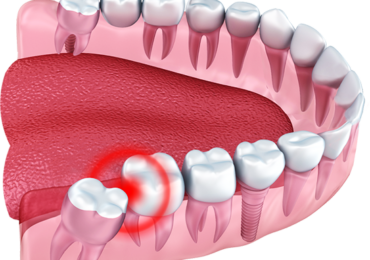
It is a procedure where a badly decayed or fractured or dead tooth is saved by removing its soft part (pulp) from the crown & the root of the tooth. Pulp is located in the core of the crown & root of the tooth. It is like mummifying a dead tooth to preserve it.
WHAT ARE THE INDICATIONS OF RCT?
- Decayed tooth
- Painful tooth
- Non-vital or dead tooth
- Trauma exposing the pulp
- Grossly attrided tooth
- Intentional RCT
HOW RCT IS DONE?
1. A Deep Infection
Root canal treatment is needed when an injury ora large cavity exposes the tooth’s pulp and the root becomes infected or inflamed.
2. Route to reach the pulp of the tooth
The dentist may numb the tooth if it is painful. An opening is made through the crown of the tooth to the pulp chamber.
3. Removing the Infected/Inflamed Tissue
Special files are used to clean the infection and unhealthy pulp is removed out of the canals. Then they shape the canals for the filling material. Irrigation is used to help clean the canals and remove debris.
4. Filling the Canals
The canals are filled with a permanent inert rubber material called gutta-percha cones. This helps to keep the canals free of infection or contamination & fills the dead space.
5. Rebuilding the tooth
A temporary filling material is placed on top of the gutta-percha to seal the opening. The filling remains until the tooth receives a permanent filling or a crown. A crown, sometimes called a cap is placed over the top of the tooth. It looks like a natural tooth.
6. Extra Support
In some cases, a post is placed into the root next to the gutta-percha. This gives the crown more support.
7. The Crowning/capping of the root canal treated tooth
To prevent the root canal treated tooth from fracture, an artificial hollow dental crown is constructed & cemented over it.
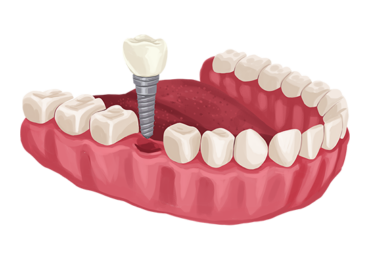
What are Dental Implants?
Dental implants are metal posts or frames that are surgically positioned into the jawbone beneath your gums. Once in place, they allow your dentist to mount replacement teeth onto them.
- Single Tooth Implants
- Multiple tooth Implants supported Bridges
- Full Mouth Rehabilitations
- Dental Implant Supported Bridges
- All on Four/six Implants supported Dentures
- Hybrid Dental Implants supported over dentures
- Bone Grafting
- Direct and Indirect Sinus Lifts
Gum Diseases (By Dr. Rajan Gupta, MDS, Periodontics)
-
- Scaling,
- Curettage,
- Gum Surgery
By Dr. Seema Gupta MDS Pedodontics
- Prophylactics,
- Interception,
- Restoration
By. Dr. Deepak Phor, MDS, Orthodontics
- Braces & Wires
Oral Surgery
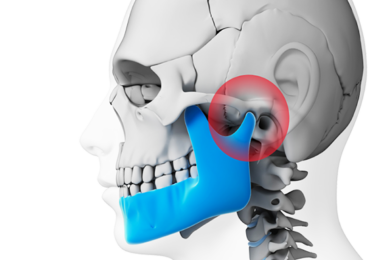
Oral and maxillofacial surgery specializes in surgery of the face, mouth, and jaws. It is an internationally recognized surgical specialty.
- Acrylic Dentures
- Flexible Dentures
- Cast partial Dentures
What is a Prosthodontist?
Prosthodontics is the dental specialty primarily concerned with the restoration and replacement of lost or damaged teeth. Sometimes called the “architects of the smile,” prosthodontists are highly trained specialists with a unique understanding of all the elements that go into a beautiful, functional and natural-looking smile—not just the teeth, but also the gums, lips, and facial features. When it comes to planning and carrying out a full-scale smile makeover, a team of dental professionals is often required; many times, that team is captained by a prosthodontist.
Dentures
Dentures are prosthetic devices constructed to replace missing teeth, and are supported by the surrounding soft and hard tissues of the oral cavity. Conventional dentures are removable. However, there are many denture designs, some which rely on bonding or clasping onto teeth or dental implants
- Acrylic Dentures
- Flexible Dentures
- Cast partial Dentures
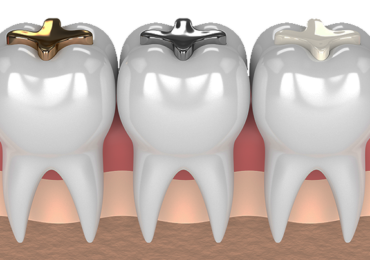
Fixed Partial Dentures
Fixed partial dentures (FPDs) are “dental prostheses that are luted, screwed, or mechanically attached or otherwise securely retained to natural teeth, tooth roots, and/or dental implant abutments.” During the past decades, many types of FPDs or “bridges” have been used to replace missing teeth. With the introduction and widespread use of osseointegrated implants, many missing teeth are now being replaced in this manner rather than with FPDs. Dental bridges can, of course, still be used successfully, and this article will briefly review the many methods of bridge construction and relate them to their applicability and current acceptance of the practicing dentist and the treated patient. These will include: cast-gold, stress-broken bridges; resin-bonded, etched retainers; porcelain-fused-to-metal (PFM) bridges; and all-ceramic bridges, including zirconia.
- Metal Crowns
- Porcelain fused to metal
- Zirconia Crowns
- Emax Crowns
- Monolith Crowns
A dental laser is a type of laser designed specifically for use in oral surgery or dentistry.
EYE Facilities Available
- 1. Complete Eye Check-up and Computer Assisted Refraction
- 2. Phacoemulsification (Stich less Cataract Surgery with Foldable Lens)
- 3. Topical Phaco (Cataract Surgery without injection)
- 4. Intraocular Lens Implant, Multifocal, IOL, Toric IOL
- 5. All types of Contact Lenses
- 6. Latest OCT
- 7. NCT (Nidek) for Comfortable early screening of Glaucoma
- 8. Pachymeter and angle evaluation for Glaucoma
- 9. Nd YAG Laser for after Cataract and Glaucoma
- 10. Optical Biometry (A Scan)
- 11. Fundus Cameras for Retinal ds
- 12. LID Surgeries, Trauma Management
- 13. Amblyopic Eye and Squint Management
- 14. Lasik surgery for Removal of Glasses
- 15. Modular OT with Zeiss Microscope and Amo Phaco Machine
- 16. Air-Conditioned Ward
Eye doctors use a wide variety of tests and procedures to examine your eyes.
These tests range from simple ones, like having you identify letters on an eye chart, to complex tests, such as using digital imaging devices to see and evaluate tiny blood vessels and other structures inside your eyes.
A comprehensive eye exam can take an hour or more, depending on the doctor and the number and complexity of tests required to fully evaluate your vision and the health of your eyes.
Here are eye and vision tests that you may encounter during a comprehensive eye exam:
- Visual acuity tests
- Color blindness test
- Cover test to check eye alignment.
- Ocular motility (eye movements) testing
- Stereopsis (depth perception) test
- Retinoscopy
- Refraction
- Autorefractors and aberrometers
- Slit lamp exam
- Glaucoma tests
- Pupil dilation
- Visual field test
Phacoemulsification
It is a modern cataract surgery in which the eye’s internal lens is emulsified with an ultrasonic handpiece and aspirated from the eye. Aspirated fluids are replaced with irrigation of balanced salt solution to maintain the anterior chamber.
Proper anesthesia is essential for ocular surgery. Topical anesthesia is most commonly employed, typically by the instillation of a local anesthetic such as tetracaine or lidocaine. Alternatively, lidocaine and/or longer-acting bupivacaine anesthestic may be injected into the area surrounding (peribulbar block) or behind (retrobulbar block) the eye muscle cone to more fully immobilize the extraocular muscles and minimize pain sensation. A facial nerve block using lidocaine and bupivacaine may occasionally be performed to reduce lid squeezing. General anesthesia is recommended for children, traumatic eye injuries with cataract, for very apprehensive or uncooperative patients and animals. Cardiovascular monitoring is preferable in local anesthesia and is mandatory in the setting of general anesthesia. Proper sterile precautions are taken to prepare the area for surgery, including use of antiseptics like povidone-iodine. Sterile drapes, gowns and gloves are employed. A plastic sheet with a receptacle helps collect the fluids during phacoemulsification. An eye speculum is inserted to keep the eyelids open.
Cataract Surgery without injection
The latest technique in cataract surgery eliminates the need for uncomfortable injection of anesthesia behind the eye and bothersome, sometimes troublesome sutures.
This is an improvement over current methods, offering the patient impressive benefits – safety, less time in surgery, relief from the usual discomfort and stress, less risk of complications and improved likelihood of success for an operation already known for its high success rate.
With this procedure, the eye is anesthetized by eye drops instead of by injection. This approach not only eliminates the uncomfortable sensation associated with injection, but also eliminates complications that can be induced by injection.
These complications are rare, but can be serious, such as permanent loss of vision, bleeding or hemorrhage behind the eye and the temporary cessation of breathing or heart beat. Omitting injection is more convenient for the patient who may be on anti-coagulation medication, and spares the patient the unpleasant experience of emerging from surgery with a “shiner”.
The incision used in the latest technique is so small that no sutures are required. Older techniques for extracapsular cataract extraction, with lens implantation, require a comparatively larger incision. Then stabilizing sutures are generally used under the muscles of the eye to hold it still for surgery.
Patients undergoing the newer procedure receive only half the normal amount of tranquilizer prior to surgery because they must cooperate with the surgeon to assure success. The patient is awake, but feels no pain when the ophthalmologist makes a tiny incision into the white part of the eye usually covered by the upper lid. Use of the eye drop therapy is possible only because of the small incision.
With the advent of cataract refractive surgery, premium intraocular lenses (IOLs) such as Toric IOLs, multifocal IOLs and accommodative IOLs are used more and more widely. Better understanding of the optics of IOLs along with improved cataract surgical techniques and devices can result in greater refractive predictability. Multifocal IOLs provide good vision at a larger range of distances than standard IOLs, improving near and distance vision simultaneously They offered a new alternative to appropriately selected patients who aspire to a spectacle-free life after their cataract removal. Meanwhile, the second generation of multifocal IOL has led to renewed interest in their use to correct refractive errors, particularly in patients who require higher levels of refractive correction and are not good candidates for corneal refractive surgery. Following bilateral multifocal IOLs implantation, rates of spectacle freedom are reported to be significantly higher (76% to 92% of patients) than with monofocal IOLs (8% to 12% of patients)
However, for cataract patients with astigmatism, multifocal IOL must be forbidden unless the astigmatism is corrected by other surgical procedure. Current options of dealing with preexisting corneal astigmatism are as followed: limbal relaxing incisions, opposite clear cornea incisions or simply the incision placement on the steep meridian. Other options include excimer laser treatment post cataract surgery or Toric IOL implantations. Among all the options, astigmatism correction with Toric IOL does not affect the cornea and make the procedure easier, it has the advantage of higher predictability and reversibility over other procedures
Although patients with unilateral astigmatism are suitable for Toric IOLs implantation in astigmatic eyes, there are still two options for their non-astigmatic eyes. One is monofocal IOLs implantation which will be a binocular monofocal consequence with a significant decrease in near vision, despite an increased distant visual acuity. Although the strategy is much more simple and easy to perform, spectacles are needed for these patients to compensate the lack of accommodation. The other is multifocal IOLs implantation, which is quite probably to bring potential benefits of compensation for pseudophakic presbyopia, binocular functional vision over a broad range of distances, and greater spectacle independence, even though it is more complicated and possible to lead to the declination of the stereopsis and contrast sensitivity.
The object of this study was to evaluate the safety and efficacy of combined implantation of multifocal and Toric monofocal IOLs in cataract patients with unilateral astigmatism.
There are two general categories of contact lenses
Soft and rigid gas permeable (RGP). All contact lenses require a valid prescription.
- Soft Contact Lenses
- Rigid Gas Permeable (RGP) Contact Lenses
- Extended Wear Contact Lenses
- Disposable (Replacement Schedule) Contact Lenses
- Lens Comparison
- Specialized Uses of Contact Lenses
- Orthokeratology (Ortho-K)
- Decorative (Plano) Contact Lenses
Optical Coherence Tomography (OCT)
Optical coherence tomography (OCT) is a non-invasive imaging test. OCT uses light waves to take cross-section pictures of your retina.
With OCT, your ophthalmologist can see each of the retina’s distinctive layers. This allows your ophthalmologist to map and measure their thickness. These measurements help with diagnosis. They also provide treatment guidance for glaucoma and diseases of the retina. These retinal diseases include age-related macular degeneration (AMD) and diabetic eye disease.
NCT (Non-Contact Tonometer) (Nidek) for Comfortable early screening of Glaucoma
This test helps diagnose glaucoma. The doctor will use a tool called a tonometer that blows a tiny puff of air, measuring eye pressure indirectly by the eye’s resistance to the puff.
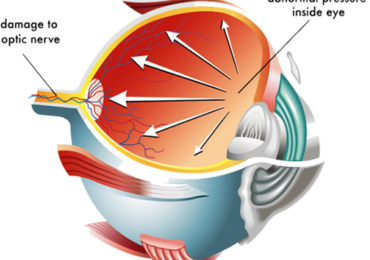
Aqueous humor is secreted by the ciliary process to the posterior chamber and goes through the pupil to the anterior chamber (inflow). It then leaves the anterior chamber through the trabecular meshwork to the venous system (outflow). Normally, there is equilibrium between inflow and outflow that creates normal intraocular pressure (IOP). Any circumstances that affect the formation of aqueous humor or outflow of aqueous humor cause changes in IOP. Local and systemic disorders, medicines, and ocular surgeries affect IOP. Higher IOP levels are associated with ganglion cell and nerve fiber layer loss. The progression of damage eventually involves the optic nerve and irreversible visual loss.
Glaucoma is the second leading cause of blindness worldwide.The only preventable risk factor for the development and progression of glaucoma is IOP. Correctly measuring IOP is very important in diagnosing glaucoma and conducting follow-ups.Medical, laser, or surgical treatments of glaucoma concentrate on lowering IOP. Earlier studies have shown that every 1 mmHg drop in IOP decreases visual field damage by 10%. Therefore, precise measurements are very important.
Pachymetry is a simple, painless test to measure the thickness of your cornea the clear window at the front of the eye. A probe called a pachymeter is gently placed on the front of the eye (the cornea) to measure its thickness. Pachymetry can help your diagnosis, because corneal thickness has the potential to influence eye pressure readings. With this measurement, your doctor can better understand your IOP reading and develop a treatment plan that is right for you. The procedure takes only about a minute to measure both eyes.
The comprehensive eye examination we describe below is recommended as a routine for all ophthalmic patients. The comprehensive eye examination helps detect not just glaucoma but other potentially blinding ocular pathology as well. Such a comprehensive eye examination comprises:
- Visual acuity and refraction,
- external examination and assessment of ocular motility,
- examination of the pupil with special attention to the presence of a relative afferent pupillary defect,
- slit-lamp biomicroscopy,
- IOP measurement,
- gonioscopy to examine the angle of the eye,
- dilated examination of the optic disc and retina and
- visual fields: If glaucoma is suspected, automated perimetry is performed to detect functional defects in the visual field.
Posterior capsule opacification or “secondary cataract” is the most common long-term complication of modern extracapsular cataract surgery. Decreased visual acuity, impaired contrast sensitivity, glare disability, and monocular diplopia are the usual visual complications secondary to posterior capsule opacification (PCO), which often require further treatment.Currently, the standard treatment for PCO is Nd:YAG laser posterior capsulotomy, which has a success rate of more than 95%.
Laser capsulotomy uses a quick-pulsed Nd:YAG laser to apply a series of focal ablations in the posterior capsule and create a small circular opening in the visual axis.Although safe and effective, the reported complications of Nd:YAG laser posterior capsulotomy include retinal detachment,cystoid macular edema (CME),and rise in IOP.
Explanations for the rise in intraocular pressure following Nd:YAG laser capsulotomy include the deposition of debris in the trabecular meshwork, trabeculitis as a consequence of the radiating “shock waves”, neurovascular mechanisms, pupillary block and inflammatory swelling of the ciliary body or iris root associated with angle-closure.
This procedure also causes a shift in the position of the implant, which can cause a change in the effective power of the lens in the eye and potentially alter the refraction of the patient. This might necessitate further refraction for the patient to ensure optimal vision. Movement and damage in the vitreous cavity and release of inflammatory mediators due to the damage of blood-aqueous barrier cause macular edema.
Retinal tears and retinal detachments too are known complications after Nd:YAG capsulotomy with rates ranging between 0% and 3.6%. The mechanism behind Nd:YAG capsulotomy leading to retinal tear and detachment is still unclear. Some postulate that rupture of the anterior vitreous hyaloid with the laser initiates a posterior vitreous detachment with subsequent retinal tear and detachment.
Fundus photography involves photographing the rear of an eye; also known as the fundus. Specialized fundus cameras consisting of an intricate microscope attached to a flash enabled camera are used in fundus photography. The main structures that can be visualized on a fundus photo are the central and peripheral retina, optic disc and macula. Fundus photography can be performed with colored filters, or with specialized dyes including fluorescein and indocyanine green.
The models and technology of fundus photography has advanced and evolved rapidly over the last century. Since the equipments are sophisticated and challenging to manufacture to clinical standards, only a few manufacturers/brands are available in the market: Welch Allyn, Digisight, Volk, Topcon, Zeiss, Canon, Nidek, Kowa, CSO, CenterVue, and Ezer are some example of fundus camera manufacturers.
Blepharoplasty (BLEF-uh-roe-plas-tee) is a type of surgery that repairs droopy eyelids and may involve removing excess skin, muscle and fat. As you age, your eyelids stretch, and the muscles supporting them weaken. As a result, excess fat may gather above and below your eyelids, causing sagging eyebrows, droopy upper lids and bags under your eyes.
Besides making you look older, severely sagging skin around your eyes can reduce your side vision (peripheral vision), especially the upper and outer parts of your field of vision. Blepharoplasty can reduce or eliminate these vision problems and make your eyes appear younger and more alert.
To help decide if blepharoplasty is right for you, find out what you can realistically expect and explore the benefits and risks of blepharoplasty.
What is Amblyopia or Lazy Eye?
Amblyopia, commonly known as lazy eye, is the eye condition noted by reduced vision not correctable by glasses or contact lenses and is not due to any eye disease. The brain, for some reason, does not fully acknowledge the images seen by the amblyopic eye. This almost always affects only one eye but may manifest with reduction of vision in both eyes. It is estimated that three percent of children under six have some form of amblyopia.
What Causes Amblyopia or a Lazy Eye?
Both eyes must receive clear images during the critical period. Anything that interferes with clear vision in either eye during the critical period (birth to 6 years of age) can result in amblyopia (a reduction in vision not corrected by glasses or elimination of an eye turn). The most common causes of amblyopia are constant strabismus (constant turn of one eye), anisometropia (different vision/prescriptions in each eye), and/or blockage of an eye due to trauma, lid droop, etc. If one eye sees clearly and the other sees a blur, the good eye and brain will inhibit (block, suppress, ignore) the eye with the blur. Thus, amblyopia is a neurologically active process. The inhibition process (suppression) can result in a permanent decrease in the vision in that eye that can not be corrected with glasses, lenses, or lasik surgery.
LASIK (laser-assisted in situ keratomileusis) is the most commonly performed laser eye surgery to treat myopia (nearsightedness), hyperopia (farsightedness) and astigmatism.
Like other types of laser refractive surgery, the LASIK procedure reshapes the front surface (cornea) of the eye to enable light entering the eye to focus on the retina without glasses or contact lenses.
LASIK typically is pain-free and requires only about 15 minutes to treat both eyes. Vision improvement is immediate and often stabilizes in as little as 24 hours.
The drive to integrate and connect a practice’s equipment is extending into the cataract suite, as well, with the recent release of integrated systems from both Alcon and Carl Zeiss Meditec. Users say the benefits can run from simply having all the patient data transferred to the operating microscope to having the microscope display digital overlays to aid in the positioning of toric lenses. Here’s a look at the two new systems and the features they bring to the practice.
Our Services
Our Patients
I am very impressed with Dr. Bansal treatment. He is well qualified & very cordial in his behavior.
Caring doctor team, He has transplaned 6 of my teeth and all are good now.
A totally hygienec hospital with full satisfaction and caring Doctor team.
Address
Yamuna Nagar –Haryana -135001 INDIA
Phone
09315555570
Email
drpunitkrbansal@gmail.com
Opening Hours
Mon-Sat: 5:00 AM – 8:30 PM
Sun: By Appointment